Vaccination progress is reshaping public health planning as governments, health agencies, clinicians, and communities track how vaccines reach people, reduce disease burden, and shape future interventions on a regional and global scale. From routine clinics to targeted outreach campaigns, this progress translates into measurable milestones for coverage and a clearer view of protection at the population level, helping policymakers, healthcare workers, and families plan safer, more effective programs. Vaccination progress statistics help explain how coverage, dose completion, and booster uptake come together to tell a practical story about risk, resilience, and everyday health, while highlighting gaps that require sustained investment. Despite strides, persistent myths require careful narrative and science-backed context, so readers can distinguish safety data from misinformation and understand real-world outcomes in diverse communities. In sum, these data-driven insights into vaccination progress illuminate benefits, risks, and the concrete steps needed to sustain momentum for communities across ages and regions.
Another way to frame the topic is by looking at how quickly vaccines are delivered and how protection propagates through communities. Public health teams track coverage growth, multi-dose completion, and program reach to gauge how well immunization campaigns are working in different settings. As these population-protection indicators rise, policymakers can tailor outreach, strengthen supply chains, and build public trust to sustain gains in protection for all ages.
1) What Vaccination Progress Reveals About Public Health
Vaccination progress is a composite measure that reflects how vaccines are reaching people, how communities accept them, and how immunization programs are integrated into routine care. It combines data from immunization records, health surveys, and national reporting to paint a broader picture of protection against disease rather than a single numeric value. By looking at trends in coverage, completion rates, and timely administration, public health officials can gauge the effectiveness of outreach and logistics across populations.
In practical terms, vaccination progress translates into fewer hospitalizations, shorter outbreak windows, and more stable healthcare systems. When progress advances, it often signals improvements in access, trust, and infrastructure—key components that determine whether vaccines meet their potential to reduce disease burden. This descriptive view helps readers understand what the numbers mean for everyday health, schools, workplaces, and vulnerable groups.
2) Immunization Rates and Coverage: From Data to Real-World Impact
Immunization rates describe the share of individuals who have received recommended vaccines, broken down by specific vaccines and by overall schedules. When we examine coverage by age and region, we can identify who is protected and where gaps persist. These metrics are essential for targeting outreach, boosting acceptance, and guiding resource allocation to communities most in need.
Beyond simple one-time measures, dose completion and booster uptake determine lasting protection. Timeliness—administering vaccines within recommended age windows—reduces vulnerability and contributes to steady, predictable public health outcomes. By framing progress through immunization rates and regional coverage, readers can connect the data to concrete actions, such as clinic accessibility, school-entry requirements, and reminder reminders for parents and caregivers.
3) Vaccination Myths Debunked: Separating Fact from Fiction
Vaccination myths debunked by science remain a focal point in health reporting, as misinformation can undermine progress even when data show clear benefits. This subheading highlights misconceptions and the robust evidence that counters them, reinforcing trust in vaccines and the public health system. By presenting the myths alongside well-designed studies, the article helps readers distinguish reliable information from fear-based claims.
Common myths—such as vaccines causing autism or containing dangerous substances—have been repeatedly tested and addressed by extensive research and regulatory review. Explaining why these claims do not hold up under scrutiny, and linking to credible sources, strengthens public understanding of how vaccines work and why misinformation can hinder vaccination progress. The goal is to replace fear with facts that support informed decisions.
4) Vaccine Safety Myths: Evidence That Supports Confidence
Vaccine safety myths can erode trust even when safety data are clear. This section emphasizes transparent testing, ongoing monitoring, and independent reviews that reassure the public about the risk-benefit balance of immunization programs. By describing how safety is evaluated—from pre-licensure trials to post-market surveillance—readers gain a practical sense of why vaccines remain among the most scrutinized medical products.
Public confidence hinges on accessible safety information and timely responses to concerns. Explaining adverse event monitoring, rare side effects, and the processes used to investigate signals helps demystify fears. When communities see open communication and rigorous oversight, they are more likely to participate in vaccination programs, supporting overall vaccination progress statistics and immunization goals.
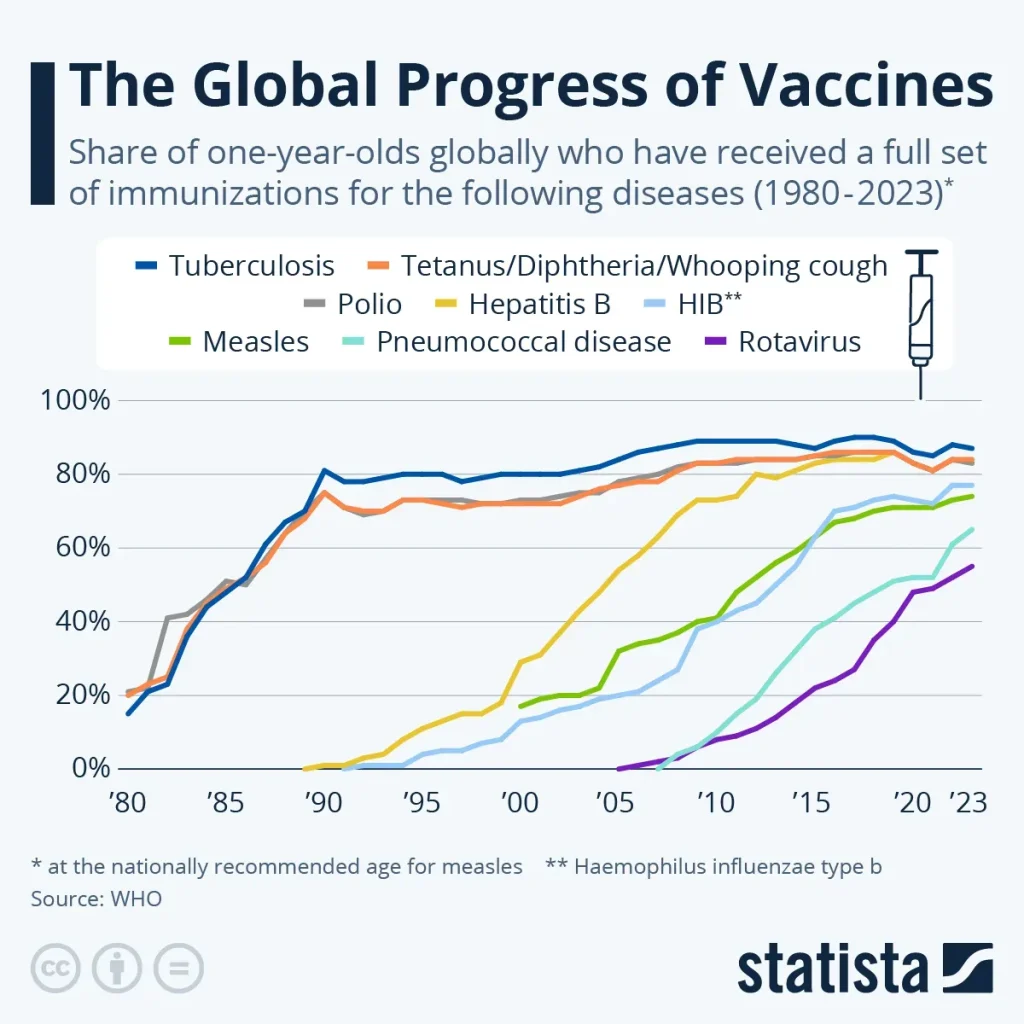
5) Vaccination Progress Statistics: Global Trends and Local Gaps
Vaccination progress statistics illuminate global trends while also spotlighting regional disparities. By aggregating data from international organizations and national ministries, analysts track shifts in coverage, dose completion, and booster uptake over time. These statistics reveal where progress is accelerating and where persistent gaps require targeted interventions.
Interpreting statistics is about more than numbers; it is about translating them into action. Regions with strong immunization programs often combine routine healthcare visits, school-based vaccination campaigns, and effective outreach to underserved populations. Conversely, indicators of low coverage point to barriers such as cold-chain challenges, access limitations, or misinformation that needs tailored communication and policy responses.
6) Herd Immunity Progress: Protecting Communities Through Vaccination
Herd immunity progress describes how population-level immunity reduces transmission and protects those who cannot be vaccinated. The degree of protection achievable depends on disease dynamics, vaccine effectiveness, and sustained vaccination coverage. Observing herd immunity progress helps public health leaders estimate outbreak risk and calibrate campaigns to maintain protective thresholds.
Continued vaccination momentum—through accessible clinics, timely boosters, and equitable distribution—advances herd immunity progress. When coverage expands across age groups and regions, vulnerable populations benefit even if they are not the primary recipients of vaccination. This forward-looking view ties vaccination effort to community resilience, outbreak prevention, and informed policy-making that supports long-term public health outcomes.
Frequently Asked Questions
What does vaccination progress mean in practical terms?
Vaccination progress is a composite measure of how widely vaccines are delivered and accepted. It includes immunization rates, dose completion, booster uptake when applicable, and the reach of programs across regions and age groups. Data from immunization records and health surveys—reported by organizations like the WHO and CDC—help track vaccination progress statistics and guide public health actions.
How do vaccination progress statistics inform public health policy?
Vaccination progress statistics identify gaps in coverage and equity, showing where improvements are needed. They help policymakers allocate resources, plan booster campaigns, adjust immunization schedules, and target outreach to underserved groups, supporting timely decisions to sustain overall vaccination progress.
Are immunization rates increasing worldwide, and what does that mean for communities?
Immunization rates vary by region, but many areas show rising coverage for key vaccines while some remain behind due to access or hesitancy. Monitoring immunization rates helps communities set priorities, strengthen health services, and reduce disease burden through targeted interventions.
What are the common vaccine safety myths, and how does debunking them affect vaccination progress?
Vaccine safety myths—such as claims of undue risk or hidden dangers—are common barriers to progress. Evidence shows vaccines are safe and continuously monitored. Vaccination myths debunked by science build public confidence and support ongoing vaccination progress.
How does herd immunity progress influence vaccination strategy?
Herd immunity progress depends on transmission dynamics and vaccine effectiveness. As vaccination progress advances and coverage increases, herd immunity progress brings fewer outbreaks and better protection for people who cannot be vaccinated.
What practical steps can communities take to improve vaccination progress?
Communities can improve vaccination progress by expanding accessibility (mobile clinics, workplace programs), conducting culturally sensitive outreach, implementing equity-driven policies, strengthening data systems for real-time monitoring, and maintaining transparent safety communication. These steps raise immunization rates, close gaps, and advance herd immunity progress.
| Aspect | Key Points |
|---|---|
| What is Vaccination Progress | A broad measure of how vaccines are delivered, accepted, and integrated into standard health care. It includes vaccination rates, completion of multi-dose schedules, booster uptake, and reach across age groups and regions. It is not a single number but a composite picture from immunization records, health surveys, and national/international reporting. |
| Why It Matters (Importance) | Vaccination progress saves lives by preventing diseases; stronger progress means lower disease incidence and hospitalizations, with less disruption to daily life. It helps identify gaps for targeted outreach and informs policy decisions on new vaccines, schedules, and booster campaigns. |
| Key Indicators | Immunization rates; Coverage by age and region; Dose completion and booster uptake; Timeliness; Equity measures. |
| Data Sources & Trends | Credible sources such as the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and national health ministries provide ongoing snapshots. Global trends show rising coverage in many regions, but progress remains uneven across countries due to resources, logistics, and messaging. |
| Regional & Global Trends | In high-income countries, routine immunization often achieves high coverage with steady booster uptake and strong surveillance. In many low- and middle-income countries, progress is significant but uneven, influenced by resources, cold-chain logistics, access, and messaging. Improvements come from stronger infrastructure, routine health visits, outbreak outreach, and school-entry vaccination requirements; pockets of under-vaccination may persist in rural or crowded urban areas or where hesitancy exists. |
| Vaccination Myths Debunked | Myth: Vaccines cause autism — thoroughly studied and debunked; no causal link. Myth: Vaccines are unsafe or contain dangerous substances — components are used in tiny, safe amounts; rigorous testing and monitoring ensure safety. Myth: Natural infection provides better immunity — infection can cause severe illness; vaccines provide protection with fewer risks. Myth: Vaccination is part of a conspiracy or coercion — programs are voluntary and based on evidence of safety and effectiveness. |
| Vaccine Safety, Efficacy & Public Confidence | Public confidence hinges on transparent safety testing, monitoring, and investigation of adverse events. Efficacy varies by disease and population, but many vaccines provide strong protection against serious outcomes. Tangible benefits (fewer hospitalizations, lower transmission) reinforce confidence and support ongoing vaccination progress. |
| Herd Immunity & Implications | Herd immunity is population-level protection achieved when transmission is reduced. Its achievable level depends on disease dynamics and vaccine effectiveness. Sustained vaccination progress moves closer to herd immunity, lowering outbreak risk and protecting vulnerable groups. |
| Maintaining Momentum: How to Improve | Accessibility (mobile clinics, workplace programs, community health centers); Outreach and education; Equity-driven policies; Robust data systems; Transparent safety communication to address concerns. |
| The Path Forward | Sustained funding, coordinated public health messaging, and adaptive strategies for new vaccines or changing disease patterns. Digital health tools, improved supply chains, and community partnerships help reach more people, improve timeliness, and boost coverage. |
Summary
Vaccination progress is a dynamic measure of how well society protects itself against preventable diseases. By analyzing immunization rates, regional coverage, and the impact of booster programs, we gain a clearer picture of where we stand and what remains to be done. Debunking myths and communicating the evidence behind vaccine safety and efficacy are essential to sustaining momentum. Observing trends over time—improving access, equity, and data-driven campaigns—helps communities stay protected. The ongoing effort requires transparent reporting, credible sources, and collaborative public health action to advance herd immunity and healthier futures for all.